NEW ORLEANS — Lawmakers could finally ban the maddening practice of surprise medical billing in Louisiana, but not without a fight from some doctors and the hospitals that hire them as independent specialists.
For the first time in 15 years, a comprehensive bill to protect patients from “balance billing” by out-of-network specialists has passed out of committee to the full state House of Representatives.
HB 283 by Rep. Raymond Crews, R-Bossier City, would require medical providers and health insurance plans to hold patients harmless for any costs charged by out-of-network providers at in-network facilities.
On the federal level, U.S. Sen. Bill Cassidy, R-La., is the lead sponsor on a bill with bipartisan support to prohibit balance billing nationwide.
According to The Commonwealth Fund, a nonprofit that advocates for affordable health care and against balance billing, 29 states have full or partial protections for consumers. Louisiana is not one of them.
Almost every year, lawmakers propose to do more, but the bills never make it out of committee.
Insurance Commissioner Jim Donelon calls balance billing a “racket” and “the greatest consumer abuse in the insurance world.” He said he tried to enforce a previous state law that banned surprise billing during emergency visits, only to have anesthesiologists, pathologists, radiologists and other ancillary providers call the law “socialist” and “un-American.” The Legislature soon repealed it.
Now, the only restriction on balance billing in Louisiana is that providers must disclose to patients that it could happen.
Crews told the House Insurance Committee on Tuesday about how little that disclosure did for him when his wife needed a procedure on her thyroid.
“When we go to check in, I make clear to the admin there, ‘Hey, I need to make sure everybody involved in this is in-network,’” Crews said. “And she told me, ‘Well, there’s no way to do that.’”
He said that refocused him on the issue, and the Insurance Committee followed his lead, passing HB 283 to the House floor on an 8-3 vote Tuesday night.
The bill is scheduled for final passage Friday. If it passes the House, it would still need Senate approval by the end of the regular session June 1.
The bill is supported by the Louisiana Association of Health Plans, a group of health insurers that often get blamed for not covering the work performed by independent contractors.
“These specialty doctors make more money being out of network than being in network and that’s because they will hound and track down the consumer using credit agencies and credit bureaus, which in this time, in our economy, can lead to bankruptcy,” said Jeff Drozda, CEO of the LAHP.
The national trade association, American Health Insurance Plans, reports that anesthesiologists, pathologists, radiologists and emergency physicians have built lucrative businesses by signing contracts with hospitals and clinics without agreeing to accept the in-network reimbursement for their services.
The AHIP said those specialists often charge between four and six times the standard Medicare reimbursement rate.
The health plan groups are backing Crews’ bill because they’re tired of being blamed for the billing practices of doctors and medical groups who won’t join their networks.
“On the front end it needs to be negotiated that if you’re going to be in this facility, you need to be in-network,” Drozda said.
But Jennifer McMahon of the Louisiana Hospital Association argued lawmakers can’t force the doctors to accept those terms.
“You’re requiring an independent business person to accept a contract that they have not negotiated,” she told the House Insurance Committee on Tuesday.
Crews’ bill also calls on hospitals to pick up the balance of any charges above the in-network rate if they hire independent specialists. That would hurt hospitals financially, especially smaller, rural ones, McMahon said.
“Of course, this is one of the key concerns for us,” she said. “For hospitals to subsidize these docs is untenable.”
Some hospitals claim to not allow balance billing but do it anyway. In 2017, Ochsner CEO Warner Thomas told WWL-TV in an interview that Ochsner facilities “make sure … if we work with a physician at one of our facilities that they’re in-network because we want to make sure our patients don’t have out-of-network costs.”
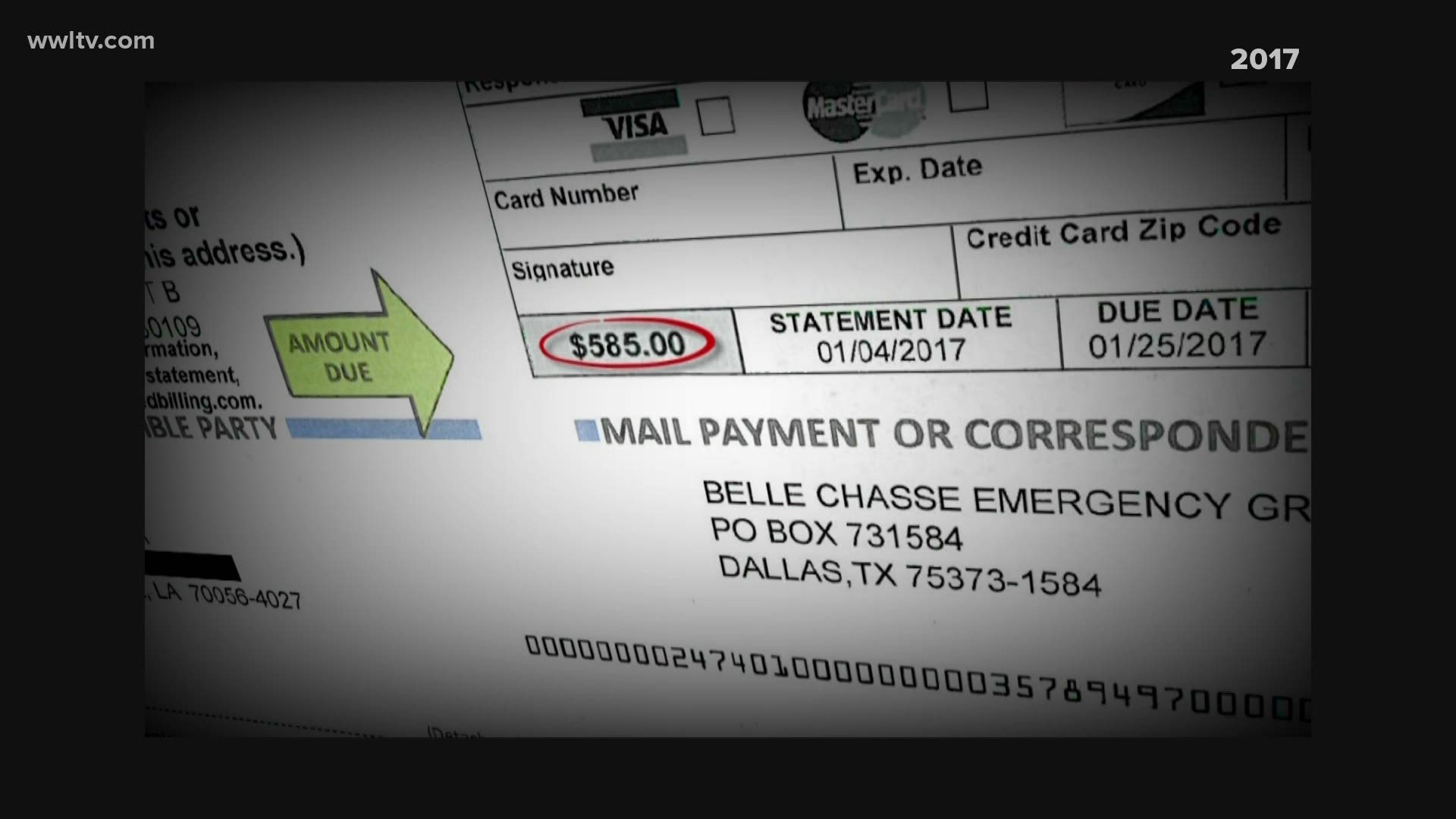
At the same time, the station told the story of Lisa Ricks, a Gretna resident who went to an in-network Ochsner emergency department and got a surprise bill for $585 from Schumacher Clinical Partners, a Lafayette-based medical group now known as SCP Health.
Four days after WWL-TV inquired about Ricks’ bill, Schumacher Clinical Partners waived all charges.
RELATED: Will reopening cause a second spike in COVID-19 cases? Louisiana's rate of infection increasing
► Get breaking news from your neighborhood delivered directly to you by downloading the FREE WWL-TV News app now in the IOS App Store or Google Play.